
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- COVID-19
- Does Diabetes Increase the Risk of Contracting COVID-19? A Population-Based Study in Korea
- Sung-Youn Chun, Dong Wook Kim, Sang Ah Lee, Su Jung Lee, Jung Hyun Chang, Yoon Jung Choi, Seong Woo Kim, Sun Ok Song
- Diabetes Metab J. 2020;44(6):897-907. Published online December 23, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0199
- 7,621 View
- 145 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study aimed to determine the infection risk of coronavirus disease 2019 (COVID-19) in patients with diabetes (according to treatment method).
Methods
Claimed subjects to the Korean National Health Insurance claims database diagnosed with COVID-19 were included. Ten thousand sixty-nine patients with COVID-19 between January 28 and April 5, 2020, were included. Stratified random sampling of 1:5 was used to select the control group of COVID-19 patients. In total 50,587 subjects were selected as the control group. After deleting the missing values, 60,656 subjects were included.
Results
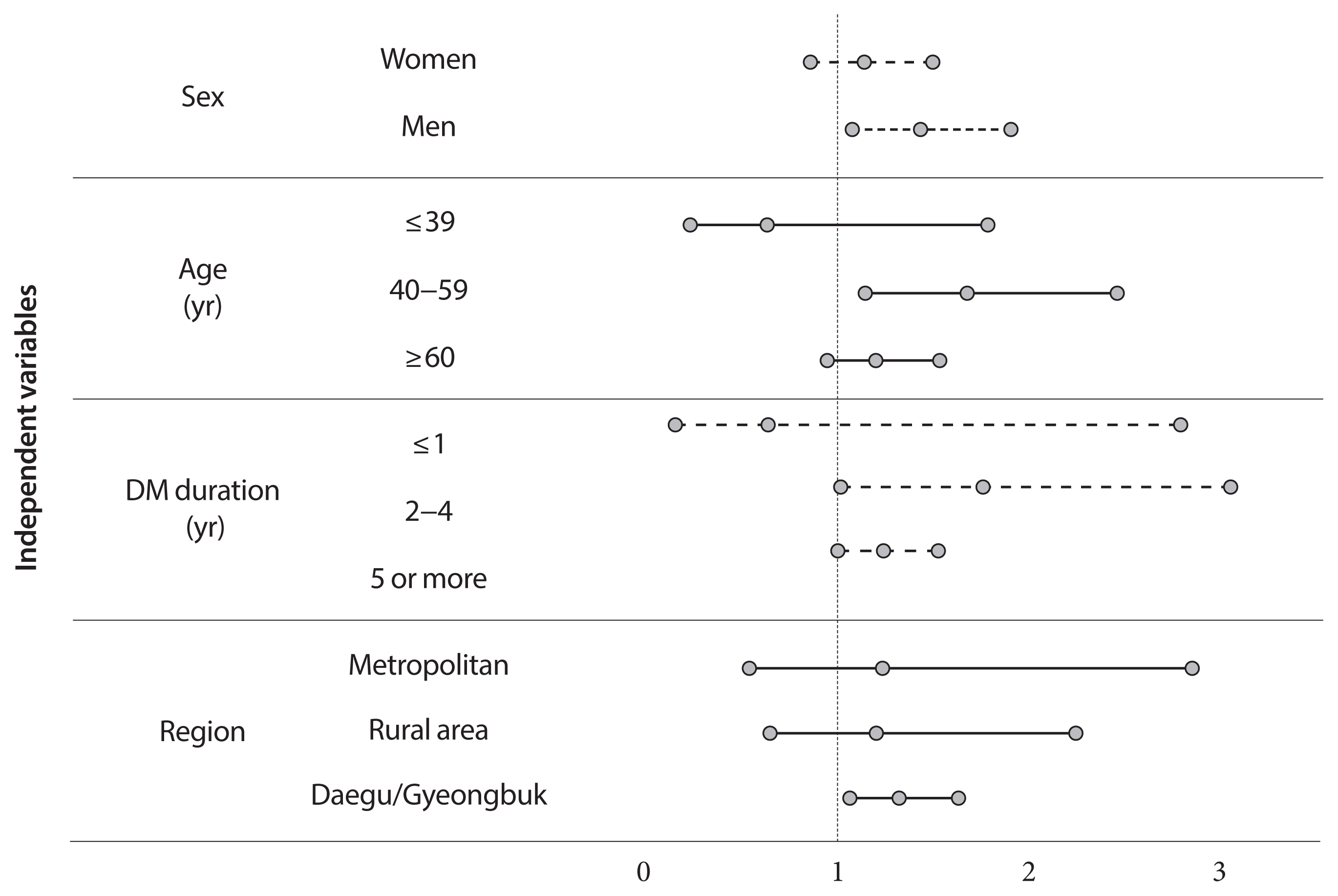
Adjusted odds ratio (OR) indicated that diabetic insulin users had a higher risk of COVID-19 than subjects without diabetes (OR, 1.25; 95% confidence interval [CI], 1.03 to 1.53; P=0.0278). In the subgroup analysis, infection risk was higher among diabetes male insulin users (OR, 1.42; 95% CI, 1.07 to 1.89), those between 40 and 59 years (OR, 1.66; 95% CI, 1.13 to 2.44). The infection risk was higher in diabetic insulin users with 2 to 4 years of morbidity (OR, 1.744; 95% CI, 1.003 to 3.044).
Conclusion
Some diabetic patients with certain conditions would be associated with a higher risk of acquiring COVID-19, highlighting their need for special attention. Efforts are warranted to ensure that diabetic patients have minimal exposure to the virus. It is important to establish proactive care and screening tests for diabetic patients suspected with COVID-19 for timely disease diagnosis and management. -
Citations
Citations to this article as recorded by- Risk factors for SARS-CoV-2 infection during the early stages of the COVID-19 pandemic: a systematic literature review
Matthew Harris, John Hart, Oashe Bhattacharya, Fiona M. Russell
Frontiers in Public Health.2023;[Epub] CrossRef - Diabetes mellitus, maternal adiposity, and insulin-dependent gestational diabetes are associated with COVID-19 in pregnancy: the INTERCOVID study
Brenda Eskenazi, Stephen Rauch, Enrico Iurlaro, Robert B. Gunier, Albertina Rego, Michael G. Gravett, Paolo Ivo Cavoretto, Philippe Deruelle, Perla K. García-May, Mohak Mhatre, Mustapha Ado Usman, Mohamed Elbahnasawy, Saturday Etuk, Raffaele Napolitano, S
American Journal of Obstetrics and Gynecology.2022; 227(1): 74.e1. CrossRef - The Role of Diabetes and Hyperglycemia on COVID-19 Infection Course—A Narrative Review
Evangelia Tzeravini, Eleftherios Stratigakos, Chris Siafarikas, Anastasios Tentolouris, Nikolaos Tentolouris
Frontiers in Clinical Diabetes and Healthcare.2022;[Epub] CrossRef - COVID-19 and Gestational Diabetes: The Role of Nutrition and Pharmacological Intervention in Preventing Adverse Outcomes
Ruben Ramirez Zegarra, Andrea Dall’Asta, Alberto Revelli, Tullio Ghi
Nutrients.2022; 14(17): 3562. CrossRef - A Comprehensive Analysis of Chinese, Japanese, Korean, US-PIMA Indian, and Trinidadian Screening Scores for Diabetes Risk Assessment and Prediction
Norma Latif Fitriyani, Muhammad Syafrudin, Siti Maghfirotul Ulyah, Ganjar Alfian, Syifa Latif Qolbiyani, Muhammad Anshari
Mathematics.2022; 10(21): 4027. CrossRef - The World-Wide Adaptations of Diabetic Management in the Face of COVID-19 and Socioeconomic Disparities: A Scoping Review
Jaafar Abou-Ghaida, Annalia Foster, Sarah Klein, Massah Bassie, Khloe Gu, Chloe Hille, Cody Brown, Michael Daniel, Caitlin Drakeley, Alek Jahnke, Abrar Karim, Omar Altabbakh, Luzan Phillpotts
Cureus.2022;[Epub] CrossRef - Dissection of non-pharmaceutical interventions implemented by Iran, South Korea, and Turkey in the fight against COVID-19 pandemic
Mohammad Keykhaei, Sogol Koolaji, Esmaeil Mohammadi, Reyhaneh Kalantar, Sahar Saeedi Moghaddam, Arya Aminorroaya, Shaghayegh Zokaei, Sina Azadnajafabad, Negar Rezaei, Erfan Ghasemi, Nazila Rezaei, Rosa Haghshenas, Yosef Farzi, Sina Rashedi, Bagher Larijan
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1919. CrossRef
- Risk factors for SARS-CoV-2 infection during the early stages of the COVID-19 pandemic: a systematic literature review
- Drug/Regimen
- Efficacy and Safety of Omega-3 Fatty Acids in Patients Treated with Statins for Residual Hypertriglyceridemia: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial
- Ji Eun Jun, In-Kyung Jeong, Jae Myung Yu, Sung Rae Kim, In Kye Lee, Kyung-Ah Han, Sung Hee Choi, Soo-Kyung Kim, Hyeong Kyu Park, Ji-Oh Mok, Yong-ho Lee, Hyuk-Sang Kwon, So Hun Kim, Ho-Cheol Kang, Sang Ah Lee, Chang Beom Lee, Kyung Mook Choi, Sung-Ho Her, Won Yong Shin, Mi-Seung Shin, Hyo-Suk Ahn, Seung Ho Kang, Jin-Man Cho, Sang-Ho Jo, Tae-Joon Cha, Seok Yeon Kim, Kyung Heon Won, Dong-Bin Kim, Jae Hyuk Lee, Moon-Kyu Lee
- Diabetes Metab J. 2020;44(1):78-90. Published online June 20, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0265
- 9,343 View
- 190 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Cardiovascular risk remains increased despite optimal low density lipoprotein cholesterol (LDL-C) level induced by intensive statin therapy. Therefore, recent guidelines recommend non-high density lipoprotein cholesterol (non-HDL-C) as a secondary target for preventing cardiovascular events. The aim of this study was to assess the efficacy and tolerability of omega-3 fatty acids (OM3-FAs) in combination with atorvastatin compared to atorvastatin alone in patients with mixed dyslipidemia.
Methods This randomized, double-blind, placebo-controlled, parallel-group, and phase III multicenter study included adults with fasting triglyceride (TG) levels ≥200 and <500 mg/dL and LDL-C levels <110 mg/dL. Eligible subjects were randomized to ATOMEGA (OM3-FAs 4,000 mg plus atorvastatin calcium 20 mg) or atorvastatin 20 mg plus placebo groups. The primary efficacy endpoints were the percent changes in TG and non-HDL-C levels from baseline at the end of treatment.
Results After 8 weeks of treatment, the percent changes from baseline in TG (−29.8% vs. 3.6%,
P <0.001) and non-HDL-C (−10.1% vs. 4.9%,P <0.001) levels were significantly greater in the ATOMEGA group (n =97) than in the atorvastatin group (n =103). Moreover, the proportion of total subjects reaching TG target of <200 mg/dL in the ATOMEGA group was significantly higher than that in the atorvastatin group (62.9% vs. 22.3%,P <0.001). The incidence of adverse events did not differ between the two groups.Conclusion The addition of OM3-FAs to atorvastatin improved TG and non-HDL-C levels to a significant extent compared to atorvastatin alone in subjects with residual hypertriglyceridemia.
-
Citations
Citations to this article as recorded by- Association Between Omega‐3 Fatty Acid Intake and Dyslipidemia: A Continuous Dose–Response Meta‐Analysis of Randomized Controlled Trials
Tianjiao Wang, Xin Zhang, Na Zhou, Yuxuan Shen, Biao Li, Bingshu E. Chen, Xinzhi Li
Journal of the American Heart Association.2023;[Epub] CrossRef - Nutraceutical support in the prevention and treatment of cardiovascular diseases
E. V. Gracheva, E. A. Starovoytova, E. S. Kulikov, N. A. Kirillova, S. V. Fedosenko, M. A. Balaganskaya, D. V. Kromka
Rational Pharmacotherapy in Cardiology.2023; 19(3): 298. CrossRef - Effect of coadministration of omega-3 fatty acids with glimepiride on glycemic control, lipid profile, irisin, and sirtuin-1 in type 2 diabetes mellitus patients: a randomized controlled trial
Rehab H. Werida, Aalaa Ramzy, Youssri Nassief Ebrahim, Maged Wasfy Helmy
BMC Endocrine Disorders.2023;[Epub] CrossRef - The Effect of Dietary Interventions on Hypertriglyceridemia: From Public Health to Molecular Nutrition Evidence
Karla Paulina Luna-Castillo, Xochitl Citlalli Olivares-Ochoa, Rocío Guadalupe Hernández-Ruiz, Iris Monserrat Llamas-Covarrubias, Saraí Citlalic Rodríguez-Reyes, Alejandra Betancourt-Núñez, Barbara Vizmanos, Erika Martínez-López, José Francisco Muñoz-Valle
Nutrients.2022; 14(5): 1104. CrossRef - The effect of omega-3 fatty acids and its combination with statins on lipid profile in patients with hypertriglyceridemia: A systematic review and meta-analysis of randomized controlled trials
Yunjiao Yang, Wen Deng, Yanmei Wang, Tongyi Li, Yiding Chen, Cong Long, Qing Wen, Yue Wu, Qiu Chen
Frontiers in Nutrition.2022;[Epub] CrossRef - Comparison of the Efficacy and Safety of Atorvastatin 40 mg/ω-3 Fatty Acids 4 g Fixed-dose Combination and Atorvastatin 40 mg Monotherapy in Hypertriglyceridemic Patients who Poorly Respond to Atorvastatin 40 mg Monotherapy: An 8-week, Multicenter, Random
Jong Shin Woo, Soon Jun Hong, Dong Hoon Cha, Kee Sik Kim, Moo Hyun Kim, Jun-Won Lee, Myung Ho Jeong, Jin-Ok Jeong, Jun-Hee Lee, Doo Soo Jeon, Eun Joo Cho, Soon Kil Kim, Jun Kwan, Chang Gyu Park, Hae Young Lee, Taek Jong Hong, Jinho Shin, Ho Joong Youn, Do
Clinical Therapeutics.2021; 43(8): 1419. CrossRef - All-Cause Mortality and Cardiovascular Death between Statins and Omega-3 Supplementation: A Meta-Analysis and Network Meta-Analysis from 55 Randomized Controlled Trials
Jeongseon Kim, Tung Hoang, Ji-Myung Kim, So Young Bu, Jeong-Hwa Choi, Eunju Park, Seung-Min Lee, Eunmi Park, Ji Yeon Min, In Seok Lee, So Young Youn, Jee-Young Yeon
Nutrients.2020; 12(10): 3203. CrossRef
- Association Between Omega‐3 Fatty Acid Intake and Dyslipidemia: A Continuous Dose–Response Meta‐Analysis of Randomized Controlled Trials
- Various Oscillation Patterns of Serum Fibroblast Growth Factor 21 Concentrations in Healthy Volunteers
- Sang Ah Lee, Eunheiu Jeong, Eun Hee Kim, Mi-Seon Shin, Jenie Yoonoo Hwang, Eun Hee Koh, Woo Je Lee, Joong-Yeol Park, Min-Seon Kim
- Diabetes Metab J. 2012;36(1):29-36. Published online February 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.1.29
- 3,670 View
- 32 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Fibroblast growth factor 21 (FGF21) was originally identified as a paroxysm proliferator activated receptor-α target gene product and is a hormone involved in metabolic regulation. The purpose of this study was to investigate the diurnal variation of serum FGF21 concentration in obese and non-obese healthy volunteers.
Methods Blood samples were collected from five non-obese (body mass index [BMI] ≤23 kg/m2) and five obese (BMI ≥25 kg/m2) healthy young men every 30 to 60 minutes over 24 hours. Serum FGF21 concentrations were determined by radioimmunoassay. Anthropometric parameters, glucose, free fatty acid, insulin, leptin, and cortisol concentrations were also measured.
Results The serum FGF21 concentrations displayed various individual oscillation patterns. The oscillation frequency ranged between 6 and 12 times per day. The average duration of oscillation was 2.52 hours (range, 1.9 to 3.0 hours). The peaks and troughs of FGF21 oscillation showed no circadian rhythm. However, the oscillation frequency had a diurnal variation and was lower during the light-off period than during the light-on period (2.4 vs. 7.3 times,
P <0.001). There was no difference in the total frequency or duration of oscillations between non-obese and obese subjects, but obese individuals had increased numbers of larger oscillations (amplitude ≥0.19 ng/mL).Conclusion Various oscillation patterns in serum FGF21 concentration were observed, and reduced oscillation frequencies were seen during sleep. The oscillation patterns of serum FGF21 concentration suggest that FGF21 may be secreted into systemic circulation in a pulsatile manner. Obesity appeared to affect the amplitude of oscillations of serum FGF21.
-
Citations
Citations to this article as recorded by- Circadian Regulation of Endocrine Fibroblast Growth Factors on Systemic Energy Metabolism
Zhenning Yang, Helmut Zarbl, Grace L. Guo
Molecular Pharmacology.2024; 105(3): 179. CrossRef - Acute sleep loss alters circulating fibroblast growth factor 21 levels in humans: A randomised crossover trial
Luiz Eduardo Mateus Brandão, Daniel Espes, Jakub Orzechowski Westholm, Teemu Martikainen, Nestori Westerlund, Lauri Lampola, Alexandru Popa, Heike Vogel, Annette Schürmann, Suzanne L. Dickson, Christian Benedict, Jonathan Cedernaes
Journal of Sleep Research.2022;[Epub] CrossRef - Metabolic Stress Index Including Mitochondrial Biomarker for Noninvasive Diagnosis of Hepatic Steatosis
Jae Seung Chang, Jhii-Hyun Ahn, Seong Hee Kang, Sang-Baek Koh, Jang-Young Kim, Soon Koo Baik, Ji Hye Huh, Samuel S. Lee, Moon Young Kim, Kyu-Sang Park
Frontiers in Endocrinology.2022;[Epub] CrossRef - Single-Arm 8-Week Ad Libitum Self-Prepared Paleo Diet Reduces Cardiometabolic Disease Risk Factors in Overweight Adults
Melissa M. Markofski, Kristofer Jennings, Chad Dolan, Natalie A. Davies, Emily C. LaVoy, Edward J. Ryan, Andres E. Carrillo
American Journal of Lifestyle Medicine.2021; 15(6): 690. CrossRef - Diurnal rhythm in clinical chemistry: An underrated source of variation
Mohamed Abou El Hassan, Edgard Delvin, Manal O. Elnenaei, Barry Hoffman
Critical Reviews in Clinical Laboratory Sciences.2018; 55(8): 516. CrossRef - Integrated stress response stimulates FGF21 expression: Systemic enhancer of longevity
Antero Salminen, Kai Kaarniranta, Anu Kauppinen
Cellular Signalling.2017; 40: 10. CrossRef - Therapeutic potential of the endocrine fibroblast growth factors FGF19, FGF21 and FGF23
Chiara Degirolamo, Carlo Sabbà, Antonio Moschetta
Nature Reviews Drug Discovery.2016; 15(1): 51. CrossRef - Response of fibroblast growth factor 21 to meal intake and insulin infusion in patients on maintenance haemodialysis
Mark Reinhard, Jan Frystyk, Bente Jespersen, Else Randers, Bo Martin Bibby, Per Ivarsen
Clinical Endocrinology.2015; 83(2): 187. CrossRef - Possible role of fibroblast growth factor 21 on atherosclerosis via amelioration of endoplasmic reticulum stress-mediated apoptosis in apoE−/− mice
Xi Wu, Yong-Fen Qi, Jin-Rui Chang, Wei-Wei Lu, Jin-Sheng Zhang, Shao-Ping Wang, Shu-Juan Cheng, Ming Zhang, Qian Fan, Yuan Lv, Hui Zhu, Man-Kun Xin, Yun Lv, Jing-Hua Liu
Heart and Vessels.2015; 30(5): 657. CrossRef - Circulating Fibroblast Growth Factors as Metabolic Regulators—A Critical Appraisal
Bo Angelin, Tobias E. Larsson, Mats Rudling
Cell Metabolism.2012; 16(6): 693. CrossRef - Metabolic actions of fibroblast growth factor 21
Daniel Cuevas-Ramos, Carlos A. Aguilar-Salinas, Francisco J. Gómez-Pérez
Current Opinion in Pediatrics.2012; 24(4): 523. CrossRef - Fibroblast Growth Factor 21: A Novel Metabolic Regulator
Ji A Seo, Nan Hee Kim
Diabetes & Metabolism Journal.2012; 36(1): 26. CrossRef - MECHANISMS IN ENDOCRINOLOGY: Biological role, clinical significance, and therapeutic possibilities of the recently discovered metabolic hormone fibroblastic growth factor 21
Pedro Iglesias, Rafael Selgas, Sara Romero, Juan J Díez
European Journal of Endocrinology.2012; 167(3): 301. CrossRef
- Circadian Regulation of Endocrine Fibroblast Growth Factors on Systemic Energy Metabolism
- The Prevalence of Peripheral Arterial Disease in Korean Patients with Type 2 Diabetes Mellitus Attending a University Hospital
- Ji Hee Yu, Jenie Yoonoo Hwang, Mi-Seon Shin, Chang Hee Jung, Eun Hee Kim, Sang Ah Lee, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Ki-Up Lee
- Diabetes Metab J. 2011;35(5):543-550. Published online October 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.5.543
- 4,273 View
- 49 Download
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Peripheral arterial disease (PAD) is a common manifestation of systemic atherosclerosis and is associated with significant morbidity and mortality. Diabetes is known to increase the risk of PAD two- to four-fold. The prevalence of PAD in Korean diabetic patients has not been established. In this study, we investigated the prevalence of PAD in Korean patients with type 2 diabetes attending a large university hospital and analyzed the factors associated with PAD.
Methods A total of 2,002 patients with type 2 diabetes who underwent ankle-brachial index (ABI) measurement in an outpatient clinic were enrolled. PAD was defined as an ABI ≤0.9. Clinical characteristics of 64 patients with PAD were compared with those of 192 age- and sex-matched control patients without PAD.
Results Of the 2,002 type 2 diabetic patients, 64 (3.2%) were diagnosed as having PAD. PAD was associated with higher prevalences of retinopathy, nephropathy, neuropathy, cerebrovascular and coronary artery disease. Patients with PAD had higher systolic blood pressure and serum triglyceride level and reported higher pack-years of smoking. Multivariate analysis showed that the presence of micro- and macrovascular complications and high systolic blood pressure are factors independently associated with PAD.
Conclusion The prevalence of PAD in diabetic patients was 3.2%, suggesting that the prevalence in Korean diabetic patients is lower than that of patients in Western countries.
-
Citations
Citations to this article as recorded by- Impaired Cardiovagal Activity as a Link Between Hyperglycemia and Arterial Stiffness in Adults With Type 2 Diabetes Mellitus Patients Among an Eastern Indian Population: A Cross-sectional Study
Nibedita Priyadarsini, Devineni Likhitha, Madumathy Ramachandran, Kishore Kumar Behera
Canadian Journal of Diabetes.2023;[Epub] CrossRef - The Predictability of Cystatin C for Peripheral Arterial Disease in Chinese Population with Type 2 Diabetes Mellitus
Luna Liu, Hai Wang, Jing Ning, Junming Han, Chunxiao Yu, Qingbo Guan, Hiroshi Okamoto
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Atherectomy in Peripheral Artery Disease: Current and Future
Yohan Kwon, Jinoo Kim, Je-Hwan Won, Seong Ho Kim, Jeong-Eun Kim, Sung-Joon Park
Journal of the Korean Society of Radiology.2021; 82(3): 551. CrossRef - Peripheral arterial disease and its correlates in patients with type 2 diabetes mellitus in a teaching hospital in northern Nigeria: a cross-sectional study
Orighomisan Freda Agboghoroma, Fatai Momodu Akemokwe, Fabian H. Puepet
BMC Cardiovascular Disorders.2020;[Epub] CrossRef - The significance of ankle-brachial index in determining peripheral artery disease in patients with type 2 diabetes mellitus over 40 years of age and the relationship of peripheral artery disease with chronic complications of diabetes
Tuğçe Nur YİĞENOĞLU, Medine KEBAPÇI, Hülya ÖZEN
Journal of Health Sciences and Medicine.2020; 3(2): 115. CrossRef - Correlation of systemic arterial stiffness with changes in retinal and choroidal microvasculature in type 2 diabetes
Mirinae Kim, Rae-Young Kim, Joo-Young Kim, Young-Hoon Park
Scientific Reports.2019;[Epub] CrossRef - Abnormally Low or High Ankle-Brachial Index Is Associated With the Development of Diabetic Retinopathy in Type 2 Diabetes Mellitus
Mei-Yueh Lee, Pi-Jung Hsiao, Jiun-Chi Huang, Wei-Hao Hsu, Szu-Chia Chen, Jer-Ming Chang, Shyi–Jang Shin
Scientific Reports.2018;[Epub] CrossRef - Peripheral Arterial Disease in Type 2 Diabetes Is Associated with an Increase in Fibrinogen Levels
Qin-Fen Chen, Dan Cao, Ting-Ting Ye, Hui-Hui Deng, Hong Zhu
International Journal of Endocrinology.2018; 2018: 1. CrossRef - Association between peripheral arterial disease and diabetic foot ulcers in patients with diabetes mellitus type 2
M.Á. Tresierra-Ayala, A. García Rojas
Medicina Universitaria.2017; 19(76): 123. CrossRef - Factors associated with lower extremity atherosclerotic disease in Chinese patients with type 2 diabetes mellitus
Qingge Gao, Binbin He, Chaoyu Zhu, Yuanyuan Xiao, Li Wei, Weiping Jia
Medicine.2016; 95(51): e5230. CrossRef - Significant interarm blood pressure difference predicts cardiovascular risk in hypertensive patients
Su-A Kim, Jang Young Kim, Jeong Bae Park
Medicine.2016; 95(24): e3888. CrossRef - 7th Asian PAD Workshop
Annals of Vascular Diseases.2016; 9(2): 135. CrossRef - 6th Asian PAD Workshop
Annals of Vascular Diseases.2015; 8(2): 135. CrossRef - Abnormally Low or High Ankle-Brachial Index Is Associated with Proliferative Diabetic Retinopathy in Type 2 Diabetic Mellitus Patients
Szu-Chia Chen, Pi-Jung Hsiao, Jiun-Chi Huang, Kun-Der Lin, Wei-Hao Hsu, Yu-Li Lee, Mei-Yueh Lee, Jer-Ming Chang, Shyi–Jang Shin, Xiao-Feng Yang
PLOS ONE.2015; 10(7): e0134718. CrossRef - Identification of peripheral arterial disease in diabetic patients and its association with quality of life, physical activity and body composition
Ana Tereza do Nascimento Sales, Guilherme Augusto de Freitas Fregonezi, Ana Gabriela Câmara Batista Silva, Cibele Teresinha Dias Ribeiro, Mario Emílio Teixeira Dourado-Junior, André Gustavo Pires Sousa, Fernando Augusto Lavezzo Dias
Jornal Vascular Brasileiro.2015; 14(1): 46. CrossRef - Chronic venous ulceration of leg associated with peripheral arterial disease: an underappreciated entity in developing country
Falguni Nag, Abhishek De, Avijit Hazra, Gobinda Chatterjee, Arghyaprasun Ghosh, Trupti V Surana
International Wound Journal.2014; 11(5): 546. CrossRef - Photoplethysmography and Continuous-Wave Doppler Ultrasound as a Complementary Test to Ankle–Brachial Index in Detection of Stenotic Peripheral Arterial Disease
Du Hyun Ro, Hyuk Ju Moon, Ji Hyeung Kim, Kyoung Min Lee, Sung Ju Kim, Dong Yeon Lee
Angiology.2013; 64(4): 314. CrossRef - Ankle brachial index as a predictor of subclinical atherosclerosis in the elderly
Ilker Tasci, Samet Verim, Hasan Kutsi Kabul, Aydogan Aydogdu
International Journal of Cardiology.2012; 160(2): 147. CrossRef - Low ankle-brachial index is an independent predictor of poor functional outcome in acute cerebral infarction
Jinkwon Kim, Dong Hyun Lee, Myoung-Jin Cha, Tae-Jin Song, Ji Hye Park, Hye Sun Lee, Chung Mo Nam, Hyo Suk Nam, Young Dae Kim, Ji Hoe Heo
Atherosclerosis.2012; 224(1): 113. CrossRef - Letter: The Prevalence of Peripheral Arterial Disease in Korean Patients with Type 2 Diabetes Mellitus Attending a University Hospital (Diabetes Metab J 2011;35:543-50)
Won Jun Kim, Cheol-Young Park
Diabetes & Metabolism Journal.2011; 35(6): 637. CrossRef
- Impaired Cardiovagal Activity as a Link Between Hyperglycemia and Arterial Stiffness in Adults With Type 2 Diabetes Mellitus Patients Among an Eastern Indian Population: A Cross-sectional Study
- Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients
- Eun Hee Kim, Ji Hee Yu, Sang Ah Lee, Eui Young Kim, Won Gu Kim, Seung Hun Lee, Eun Hee Cho, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Ki-Up Lee
- Korean Diabetes J. 2010;34(2):95-100. Published online April 30, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.2.95
- 4,427 View
- 31 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Serum cystatin C level is a more sensitive marker of renal dysfunction than serum creatinine level. Serum cystatin C level was recently reported to predict the development of cardiovascular disease. This study was performed to evaluate whether the cystatin C level is associated with coronary artery disease (CAD), independent of diabetic nephropathy.
Methods We conducted a case-control study to assess the relationship between serum cystatin C level and coronary artery disease in diabetic patients. Among 460 diabetic patients, 38 diabetic patients had CAD. The control group consisted of 38 diabetic patients who were matched to cases by age, sex, and presence/absence of diabetic nephropathy. Serum cystatin C level was measured in stored samples.
Results Serum cystatin C level was significantly higher in patients with diabetic nephropathy, both in CAD and non-CAD patients. However, serum cystatin C level did not differ between CAD and non-CAD patients, regardless of diabetic nephropathy.
Conclusion Serum cystatin C level is a marker of renal dysfunction, but not coronary artery disease, in diabetic patients.
-
Citations
Citations to this article as recorded by- Higher Levels of Cystatin C in HIV/AIDS Patients with Metabolic Syndrome
Gordana Dragović, Danica Srdić, Khawla Al Musalhi, Ivan Soldatović, Jovana Kušić, Djordje Jevtović, Devaki Nair
Basic & Clinical Pharmacology & Toxicology.2018; 122(4): 396. CrossRef - The association between serum cystatin C and carotid intima–media thickness in metabolic syndrome patients with normal estimated glomerular filtration rate
Rong Huang, Jingli Gu, Qin Cao, Jiahua Ma, Weiwei Gu, Zhuping Fan
Clinica Chimica Acta.2015; 448: 170. CrossRef - Association of plasma cystatin C levels with angiographically documented coronary artery disease in patients of Indian origin
Aditya Batra, Aditya Kapoor, R.K. Sharma, Nitin Agrawal, Archana Sinha, Sudeep Kumar, Naveen Garg, Satyendra Tewari, Pravin K. Goel
Journal of Cardiology.2012; 59(2): 182. CrossRef - Cystatin C and asymptomatic coronary artery disease in patients with metabolic syndrome and normal glomerular filtration rate
Xie Qing, Wang Furong, Liu Yunxia, Zhang Jian, Wang Xuping, Gao Ling
Cardiovascular Diabetology.2012;[Epub] CrossRef - Response: Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients (Korean Diabetes J 2010;34:95-100)
Eun Hee Kim, Ki-Up Lee
Korean Diabetes Journal.2010; 34(3): 209. CrossRef - Serum Cystatin C as a Biomarker for Predicting Coronary Artery Disease in Diabetes
Jee-Young Oh
Korean Diabetes Journal.2010; 34(2): 84. CrossRef - Letter: Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients (Korean Diabetes J 2010;34:95-100)
Kyu-Chang Won
Korean Diabetes Journal.2010; 34(3): 207. CrossRef
- Higher Levels of Cystatin C in HIV/AIDS Patients with Metabolic Syndrome
- Nitric Oxide Increases Insulin Sensitivity in Skeletal Muscle by Improving Mitochondrial Function and Insulin Signaling.
- Woo Je Lee, Hyoun Sik Kim, Hye Sun Park, Mi Ok Kim, Mina Kim, Ji Young Yun, Eun Hee Kim, Sang Ah Lee, Seung Hun Lee, Eun Hee Koh, Joong Yeol Park, Ki Up Lee
- Korean Diabetes J. 2009;33(3):198-205. Published online June 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.3.198
- 2,096 View
- 22 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Accumulating evidence has suggested that nitric oxide (NO) is involved in the regulation of insulin sensitivity in skeletal muscle. Recent studies also suggested NO as an important molecule regulating mitochondrial biogenesis. This study examined the effect of the NO donor, 3-morpholinosydnonimine (SIN-1), on glucose metabolism in skeletal muscle and tested the hypothesis that NO's effect on glucose metabolism is mediated by its effect on mitochondrial function. METHODS: In Sprague-Dawley (SD) rats treated with SIN-1 for 4 weeks, insulin sensitivity was measured by a glucose clamp study. Triglyceride content and fatty acid oxidation were measured in the skeletal muscle. In addition, mitochondrial DNA content and mRNA expression of mitochondrial biogenesis markers were assessed by real-time polymerase chain reaction and expression of insulin receptor substrate (IRS)-1 and Akt were examined by Western blot analysis in skeletal muscle. In C2C12 cells, insulin sensitivity was measured by 2-deoxyglucose uptake and Western blot analysis was used to examine the expression of IRS-1 and Akt. RESULTS: SIN-1 improved insulin sensitivity in C2C12 cells and skeletal muscles of SD rats. In addition, SIN-1 decreased triglyceride content and increased fatty acid oxidation in skeletal muscle. Mitochondrial DNA contents and biogenesis in the skeletal muscle were increased by SIN-1 treatment. Moreover, SIN-1 increased the expression of phosphor-IRS-1 and phosphor-Akt in the skeletal muscle and muscle cells. CONCLUSION: Our results suggest that NO mediates glucose uptake in skeletal muscle both in vitro and in vivo by improving mitochondrial function and stimulating insulin signaling pathways. -
Citations
Citations to this article as recorded by- NO-Rich Diet for Lifestyle-Related Diseases
Jun Kobayashi, Kazuo Ohtake, Hiroyuki Uchida
Nutrients.2015; 7(6): 4911. CrossRef - Metformin Activates AMP Kinase through Inhibition of AMP Deaminase
Jiangyong Ouyang, Rahulkumar A. Parakhia, Raymond S. Ochs
Journal of Biological Chemistry.2011; 286(1): 1. CrossRef
- NO-Rich Diet for Lifestyle-Related Diseases
- Anti-GAD Antibody in Patients with Adult-Onset Diabetes in Korea.
- Sang Ah Lee, Eui Young Kim, Eun Hee Kim, Ji Yun Jeong, Eun Heui Jeong, Dong Woo Kim, Eun Hee Cho, Eun Hee Koh, Min Seon Kim, Joong Yeol Park, Ki Up Lee
- Korean Diabetes J. 2009;33(1):16-23. Published online February 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.1.16
- 2,349 View
- 23 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It is well known that the clinical characteristics of diabetes mellitus in Korean people are different from those of Western people. The purpose of this study was to investigate the prevalence of the anti-GAD antibody (GADA) in a large number of Korean patients with adult-onset diabetes. METHODS: The GADA was measured by radioimmunoassay for 11,472 adult-onset diabetic patients who visited the Asan Medical Center from 1998 to 2007. According to the fasting C-peptide levels, we classified the patients into an insulin dependent diabetes mellitus group (IDDM; C-peptide < 0.6 ng/mL) and non-insulin dependent diabetes mellitus group (NIDDM; C-peptide > or = 1.0 ng/mL). Other clinical and laboratory data were obtained from medical records. RESULTS: Among the 11,147 diabetic patients, 9,250 patients were classified as NIDDM, 922 patients were classified as IDDM and 975 patients excluded. Within the latter group 472 patients were to absolute insulin deficient (C-peptide < 0.1 ng/mL). The prevalence of GADA was 22.0% in the IDDM group and 4.7% in the NIDDM group. GADA was more prevalent in younger-onset NIDDM patients (25~40 years of age; 12.4%) than in older-onset NIDDM patients (> or = 40 years of age; 3.8%). The GADA-positive NIDDM patients had lower C-peptide and BMI levels, and higher rates of typical diabetic symptoms and insulin treatment. CONCLUSION: The prevalence of GADA in Korean patients with IDDM and NIDDM was lower than that reported in Western populations. It is thus suggested that autoimmunity is a rarer cause of diabetes in Korean people. However, since over 10% of younger-onset NIDDM patients were positive for GADA, routine GADA measurement in such patients is recommended. -
Citations
Citations to this article as recorded by- Distinct changes to pancreatic volume rather than pancreatic autoantibody positivity: insights into immune checkpoint inhibitors induced diabetes mellitus
Hung-Hui Wei, Ying-Chieh Lai, Gigin Lin, Cheng-Wei Lin, Ya-Chu Chang, John Wen-Cheng Chang, Miaw-Jene Liou, I-Wen Chen
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - Recent information on test utilization and intraindividual change in anti-glutamic acid decarboxylase antibody in Korea: a retrospective study
Rihwa Choi, Wonseo Park, Gayoung Chun, Jiwon Lee, Sang Gon Lee, Eun Hee Lee
BMJ Open Diabetes Research & Care.2022; 10(3): e002739. CrossRef - The effect of glargine versus glimepiride on pancreatic β-cell function in patients with type 2 diabetes uncontrolled on metformin monotherapy: open-label, randomized, controlled study
Jun Sung Moon, Kyoung Soo Ha, Ji Sung Yoon, Hyoung Woo Lee, Hyun Chul Lee, Kyu Chang Won
Acta Diabetologica.2014; 51(2): 277. CrossRef - Successful treatment of latent autoimmune diabetes in adults with Traditional Chinese Medicine: a case report
Jiaxing Tian, Wenke Liu, Zhong Zhen, Xiaolin Tong
Journal of Traditional Chinese Medicine.2013; 33(6): 766. CrossRef - The prevalence and characteristics of latent autoimmune diabetes in adults (LADA) and its relation with chronic complications in a clinical department of a university hospital in Korea
Mi-Oh Roh, Chan-Hee Jung, Bo-Yeon Kim, Ji-Oh Mok, Chul-Hee Kim
Acta Diabetologica.2013; 50(2): 129. CrossRef - Prevalence and Clinical Characteristics of Recently Diagnosed Type 2 Diabetes Patients with Positive Anti-Glutamic Acid Decarboxylase Antibody
Yul Hwangbo, Jin Taek Kim, Eun Ky Kim, Ah Reum Khang, Tae Jung Oh, Hak Chul Jang, Kyong Soo Park, Seong Yeon Kim, Hong Kyu Lee, Young Min Cho
Diabetes & Metabolism Journal.2012; 36(2): 136. CrossRef - Body Composition Analysis in Newly Diagnosed Diabetic Adolescent Girls
Yong Hyuk Kim, Min Kyoung Song, Sochung Chung
Journal of Korean Society of Pediatric Endocrinology.2011; 16(3): 172. CrossRef - Increasing Trend in the Number of Severe Hypoglycemia Patients in Korea
Jin Taek Kim, Tae Jung Oh, Ye An Lee, Jun Ho Bae, Hyo Jeong Kim, Hye Seung Jung, Young Min Cho, Kyong Soo Park, Soo Lim, Hak Chul Jang, Hong Kyu Lee
Diabetes & Metabolism Journal.2011; 35(2): 166. CrossRef - Progression to insulin deficiency in Korean patients with Type 2 diabetes mellitus positive for anti‐GAD antibody
S. A. Lee, W. J. Lee, E. H. Kim, J. H. Yu, C. H. Jung, E. H. Koh, M.‐S. Kim, J.‐Y. Park, K.‐U. Lee
Diabetic Medicine.2011; 28(3): 319. CrossRef - Anti-GAD Antibody in Patients with Adult-Onset Diabetes in Korea
Eun-Gyoung Hong
Korean Diabetes Journal.2009; 33(1): 13. CrossRef
- Distinct changes to pancreatic volume rather than pancreatic autoantibody positivity: insights into immune checkpoint inhibitors induced diabetes mellitus

 KDA
KDA
 First
First Prev
Prev





